The future of ophthalmology is looking promising with the development of new technologies and treatments that are aimed at improving the diagnosis and treatment of eye diseases. Here are a few areas where advancements are being made:
Artificial intelligence
Artificial intelligence (AI) is being used to analyze large amounts of data from images and medical records, and to assist in the diagnosis of eye diseases. AI algorithms can be trained to identify and monitor ocular conditions and diseases, such as age-related macular degeneration, diabetic retinopathy, and glaucoma, by analyzing medical images, including optical coherence tomography (OCT) scans and retinal photographs. AI algorithms can be more accurate and faster at identifying these conditions compared to traditional methods.
Telemedicine
Telemedicine technology is being used to remotely diagnose and monitor eye diseases, making eye care more accessible to patients in remote or underserved areas.
Stem cell therapy
Stem cell therapy is being researched as a potential treatment for eye diseases such as age-related macular degeneration and retinal detachment. Ophthalmologists are making great strides in the field of stem cell therapy. Stem cells have been used to treat a variety of ocular conditions, including age-related macular degeneration (AMD), retinal degeneration (RD), corneal damage (CD), and more, due to their potential to repair and regenerate damaged eye tissue. Because it may help people with these conditions regain their sight, it could revolutionize the ophthalmology field. Stem cell therapy has shown promise in the treatment of a variety of conditions, but more study and testing are needed to ensure its safety and effectiveness before it can be used on a large scale.
Gene therapy:
Gene therapy is being researched as a potential treatment for inherited eye diseases such as retinitis pigmentosa and Leber’s congenital amaurosis.
Ophthalmic gene therapy is a developing field with the potential to eradicate several hereditary retinal disorders. This is accomplished by inserting a functional copy of the defective gene into the eye’s cellular DNA, thus fixing the underlying genetic defect and reestablishing normal cellular function.
Clinical trials of gene therapy to treat retinal diseases, such as Leber congenital amaurosis and x-linked retinitis pigmentosa, have yielded encouraging results. Patients’ vision has improved, and in some cases they’ve gained significant functional vision, in these studies.
Gene therapy’s potential to cure inherited retinal diseases has sparked considerable excitement in the ophthalmology field, despite the technology’s infancy. Gene therapy shows great promise as a treatment option for people with retinal diseases, but more research and clinical trials are needed to evaluate its safety and efficacy.
Surgical techniques
Advancements in surgical techniques such as laser surgery and minimally invasive surgery are helping to improve the outcomes of eye surgeries.
3D printing
3D printing technology is being used to create customized implants, prosthetics and surgical tools for eye surgeries.
Biomaterials
Biomaterials are being used to create new types of contact lenses and artificial corneas that can improve the vision of patients with eye diseases.

Bionic Eyes
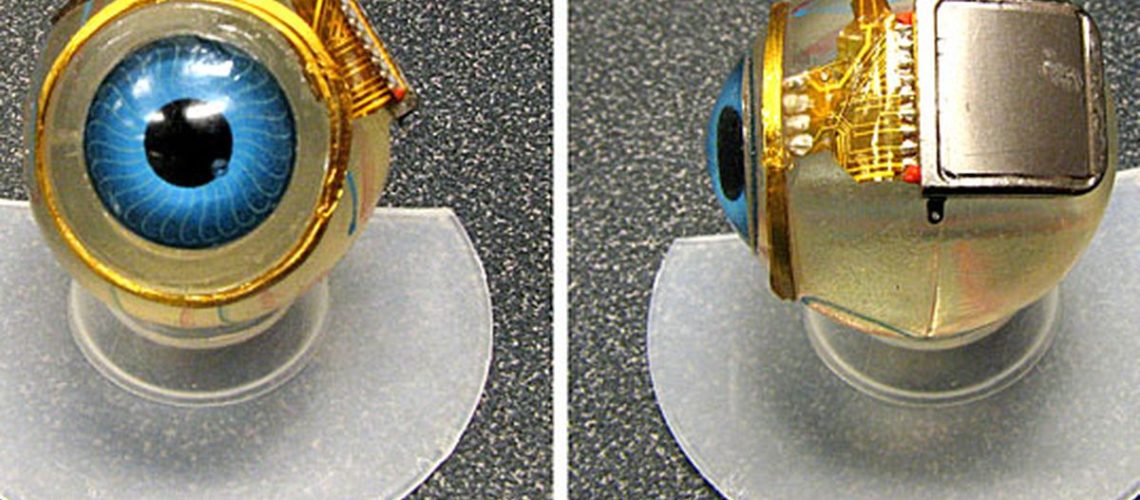
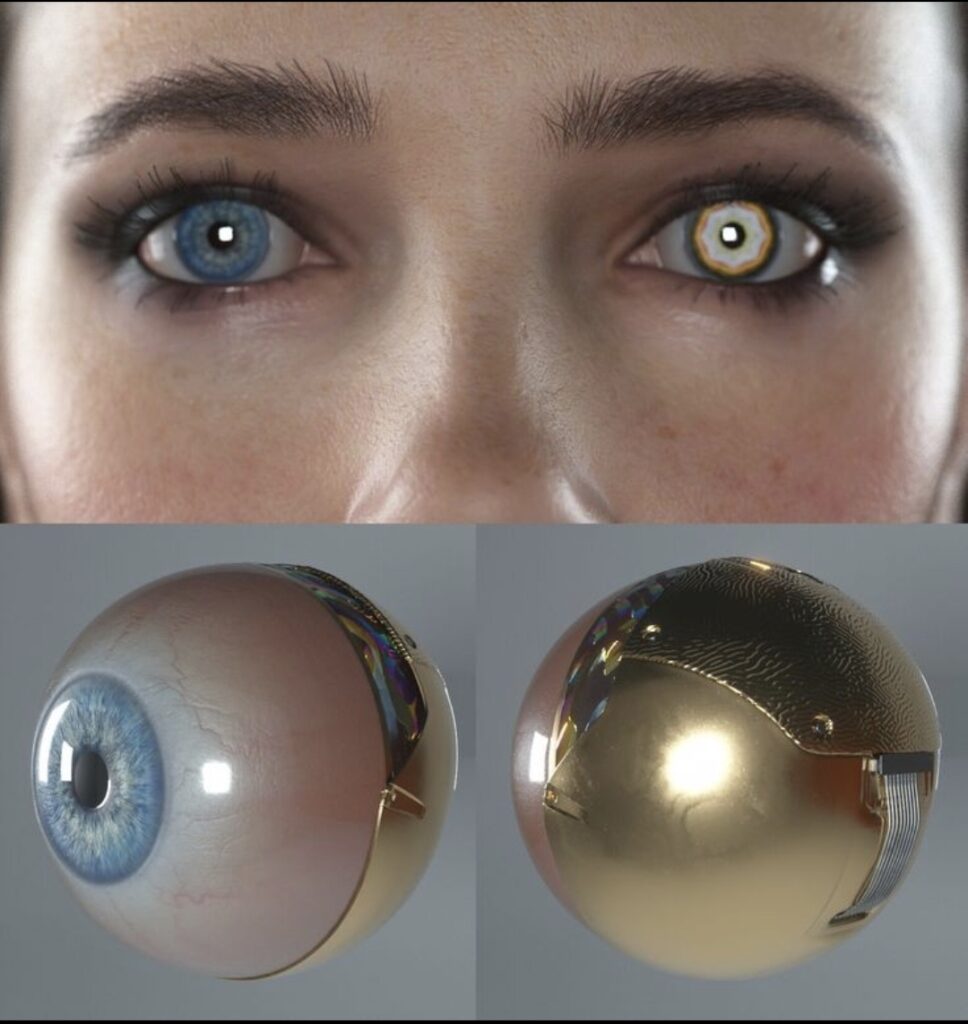
People who have lost their sight may be able to see again with the help of bionic eyes. They use a system of cameras, computer processors, and electrodes implanted in the retina to perform visual tasks in a manner similar to the human eye. Electrical signals produced by the camera and processor are received by the electrodes, stimulating the retina and conveying visual information to the brain.
Bionic eyes are not a new idea; scientists have been studying them for decades. However, these devices have come a long way in recent years, making them more useful and affordable for those who could benefit from them.
Second Sight Medical Products’ Argus II Retinal Prosthesis System is one of the most promising bionic eyes on the market right now. This system consists of a pair of glasses equipped with a camera that transmits data to a processor worn at the waist. Electrodes implanted in the retina are stimulated by the processor, which in turn sends visual information to the brain.
The German firm Retina Implant AG has also created a bionic eye called the Alpha IMS. The photoreceptor cells in the retina are what convert light into electrical signals that are sent to the brain; this device is meant to replace damaged or missing photoreceptor cells. The Alpha IMS system includes a tiny camera built into a pair of glasses and a microchip implanted directly into the retina. The visual data is captured by the camera and transmitted to the microchip, which then stimulates the retina and relays the data to the brain.
Bionic eyes have the potential to revolutionize medicine and open up new possibilities for the treatment of vision loss, in addition to the practical benefits they can provide. Additional sensors, such as temperature or pressure sensors, could be built into future bionic eyes to help users better detect obstacles or navigate new environments, for example.
In addition, bionic eyes could be programmed with AI systems to learn the user’s visual preferences and habits, allowing them to tailor their experience and make suggestions based on past visual data. The artificial intelligence in a bionic eye, for instance, could study the user’s visual habits and make recommendations for improving their eyesight.
Despite all the promise, there are still obstacles to overcome before bionic eyes become commonplace. Since bionic eyes are still quite pricy, many people in need of them may be unable to afford them. The need for more clinical trials to confirm their safety and efficacy and show that they are adaptable for use in different populations is another obstacle.
It’s worth noting that the development and implementation of these new technologies and treatments will depend on the availability of funding and the regulatory approval process. Also, the COVID-19 pandemic has impacted ophthalmology in many ways, such as the decrease of surgeries, that have been postponed due to the priority of emergency cases, and the increase of virtual consultations, which might continue in the future.