The retina is a thin, transparent, and delicate sensory membrane located at the back of the eye. It is constituted by an expansion of the optic nerve. The retina detects light and converts it into signals that are sent to the optic nerve by nerve impulses that are propagated by a sensitive bioelectric current.
The retina is made up of 10 layers intimately connected but well-differentiated. It is made up of photoreceptors (rods and cones). The cones: they work with a lot of light, they help us to see during the day and they are in charge of color vision. The rods: are activated by darkness and are responsible for our night vision.
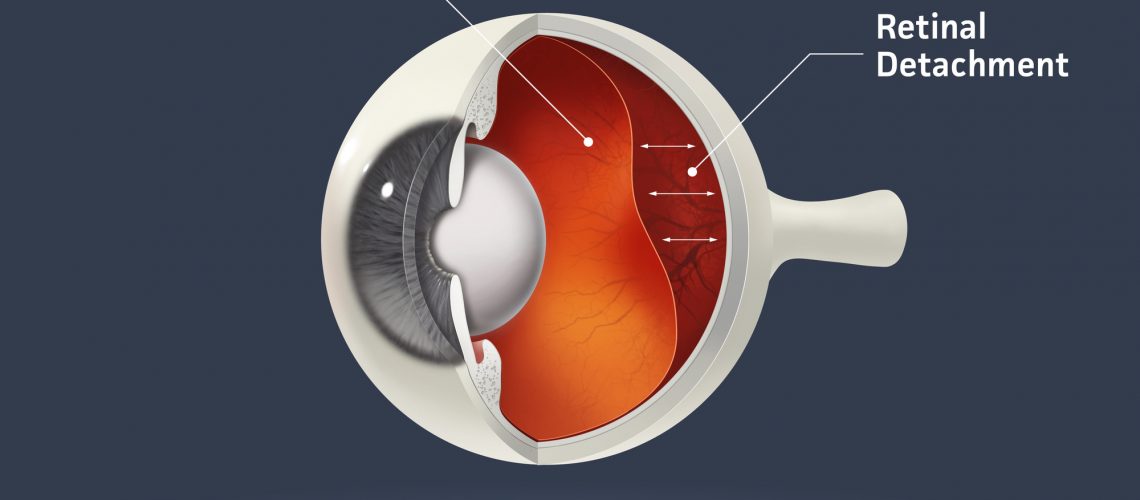
Retinal detachment is when the retina separates from the back of the eye and there is considerable loss of vision. The detachment causes the appearance of a dark cloud or fabric in the vision, depending on the degree of extension and the area of the detachment.
Due to the sensitivity and delicacy of the retina, any detachment is considered an emergency: the faster it is attended by a retinologist, the higher the chances of preserving and recovering vision.
Risk factor’s:
- High myopia
- Eye trauma.
- Uveitis.
- Diving to extreme depths.
- Posterior vitreous detachment.
- Weak areas of the retina
- Complications in eye surgeries.
- Holes and tears in the retina are considered to be the main factor in the production and persistence of the detachment, allowing vitreous fluid to leak freely into the retina.
Symptoms:
- Flickering light flashes
- Many floaters in view (vitreous floaters)
- Dark shadow on the periphery of vision
- A gray curtain that covers part of the visual field.
Retinal detachment is diagnosed by dilating the pupils of the affected eye and evaluating the fundus by an ophthalmologist. Retinal detachment is treated by a retinologist, through surgeries called vitrectomy, pneumatic retinopexy and scleral loop. During vitrectomy, the vitreous is replaced by a bubble of air, gas, or oil. The bubble pushes the retina back into place to heal properly. If an oil bubble is used, the ophthalmologist will remove it a few months later.
You cannot travel to high altitudes or dive if an air or gas bubble has been placed in you.
This is because a change in altitude causes the gas to expand and increase eye pressure.
What to expect after surgery:
- You will need to wear an eye patch after surgery.
- You may feel some discomfort for a few days after surgery.
- You should rest and be less active after surgery for a few weeks. Your ophthalmologist will tell you when you can safely return to exercise, driving, and other activities.
- If you have had a bubble placed in your eye, you will need to hold your head in a certain position for a period of time. Your retina specialist will tell you in which specific position. It is very important to follow the instructions so that your eye heals well and your vision returns.
- You may see floaters, lights, or flickering bubbles for a few weeks after surgery.
- Vision should begin to improve approximately four to six weeks after surgery.
- The retina may continue to heal for a year or more after surgery. The improvement in vision depends on the damage that the detachment has caused to the cells of the retina.
Your ophthalmologist/retinologist should explain the risks and how surgery can benefit you.
If you suspect having retina detachment, seek for help inmeadiately.